Getting to the bottom of bowel cancer

In an anonymous looking room in the grounds of St James’s Hospital in Leeds, Professor Philip Quirke is just getting into his stride.
The head of pathology and tumour biology has just been awarded £1.5m of funding by Yorkshire Cancer Research. The money will allow the team at Leeds University to continue their research into bowel cancer and Prof Quirke is keen to talk about the past successes which have made this latest grant possible.
Advertisement
Hide AdAdvertisement
Hide AdLater there will be a PowerPoint presentation he’s prepared, but first there’s a quick demonstration of a model of a human bowel. It was made by a 3D printer and is evidence of just how much has changed in modern medicine. The models allow the team to examine in detail how successful surgery to remove a tumour has been and it’s the kind of digital technology which has been quietly pioneered in this corner of the teaching hospital. It’s all clever stuff, but the lynchpin to the improvements made at Leeds is in fact more than a century old.
“It’s fair to say that we have gone back to basics,” says Prof Quirke, who admits that when he first began his research bowel cancer was a much overlooked disease. In some quarters it still is. “Over the years different surgeons adopted different techniques when it came to operating on bowel cancer tumours. However, the best practice would seem to be the method which was described in a textbook back in 1909.
“With something like bowel cancer you basically have one chance to get it right. If you don’t remove all the tumour it will likely spread to the nerve endings where it is then impossible to treat. At that point all you can do is provide palliative care.”
Every year around 41,000 people in the UK are diagnosed with bowel cancer. It is the fourth most common form of the disease and annually claims the lives of 16,000 people.
Advertisement
Hide AdAdvertisement
Hide AdThe work already done at Leeds has shown removing more of the tissue during initial surgery could increase survival rates by 15 per cent, saving the lives of 5,000 a year. It’s an impressive result and one which requires no expensive drugs - always a bonus for a cash-strapped NHS - but Prof Quirke admits it hasn’t always been an easy sell.
“No surgeon likes to be told the way they have been doing things is wrong and yes, there has been some resistance, but the evidence is there,” he says. “Surgery is a craft, it’s a bit like woodwork but if you are trained badly those bad habits will stay with you throughout your career. Our aim is to save patients lives and if that means a few awkward conversations with surgeons, well, so be it.”
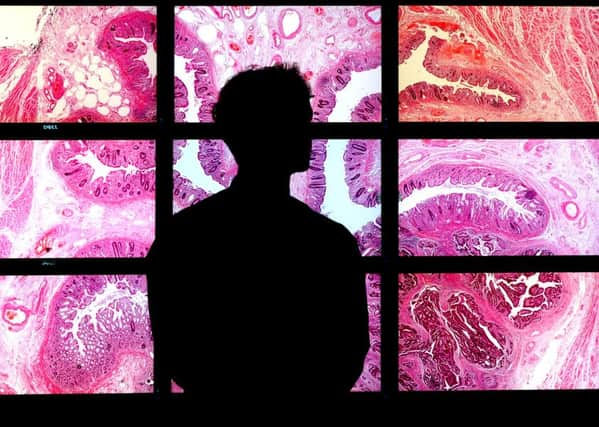
The team at Leeds has made great strides. After more than 15 years studying photographic records of tumours removed in Leeds and around the world in order to compare different types of surgery they believe they have hit on the best practice.
The technique has been used in a number of centres in Germany, Japan and Denmark and in each case the outcomes have been proven to be better. Ultimately, Prof Quirke would like to see all surgeons responsible for bowel cancer operations trained in exactly the same way.
Advertisement
Hide AdAdvertisement
Hide AdAt the moment there are significant variations and changes to who can and can’t access patient records means monitoring individual surgeons is all but impossible. Previously, Prof Quirke would have been able to look at the success rates for every surgeon in every hospital across the country. He and his team would have been able to identify those who had the best outcomes and those whose patients fared worst. However, that changed amid fears patient information was in danger of being sold off to pharmaceutical giants and insurance companies.
“There was an issue about security, but the response went too far. I don’t suppose anyone ever intended it to have an impact on genuine medical research, but that’s what has happened,” says Prof Quirke. “The reality is that two per cent of all doctors are mad, bad or alcoholic - that’s exactly the same percentage as the general population, but surely we should be actively identifying who those rogue professionals are and the current regulations make that very difficult.
“Differences in outcomes still exist even within Yorkshire Hospitals as does the treatment offered to each individual patient. Doctors interpret the disease differently and some lack an understanding of its history and response to radiotherapy and chemotherapy. We have made great strides in improving outcomes for people with bowel cancer and survival rates increase year on year, but there is still room for improvement.”
The exact cause of bowel cancer is not known, but 85 out of every 100 cases is diagnosed in patients aged 60 an over. As with most cancers, with early treatment key, the Leeds team has also played a key role in the roll out of a screening programme.
Advertisement
Hide AdAdvertisement
Hide Ad“For some cancers the value of mass screening is debatable, but when you talk about bowel cancer it absolutely works,” says Prof Quirke. “Currently every one over 60 is sent a home test kit and given that it’s not necessarily the most pleasant of things to do, the 55 per cent take up is pretty good.
“Screening is incredibly effective at detecting the disease long before any physical symptoms appear and it’s something that we do really need to push.”
The latest grant from YCR will allow Prof Quirke to continue clinical trials looking at the impact of surgery, radiotherapy and chemotherapy on bowel cancer patients and allow them to test new methods of treatment which might further boost survival rates.
“We are in a unique position to improve outcomes as we have created the largest collection of bowel cancer trial patients in the world,” he says. “As with many other diseases historically there was a tendency to think that there was only one right way to treat a patient. However, what we are exploring now is much more personalised treatment.
Advertisement
Hide AdAdvertisement
Hide Ad“Some people might benefit from a round of chemotherapy before surgery, others might not and it’s by exploring those detailed differences between tumours that we can really begin to transform patient outcomes.”
The money the Leeds team has just been awarded from YCR should also unlock other potential funding streams allowing the increase the pot by 10 or 15 times the initial grant.
“In medical research terms £1.5m might not sound like a huge amount, but the ripple effect is immense,” says Prof Quirke. “With the backing of the YCR it becomes much easier to secure other investment and that’s not just good for us, but it’s good for the city.
“Biomedical science is a real growth area for Leeds. It creates high quality jobs and means that good people don’t have to go to London to fulfil their career ambitions. It really is a win win situation.”